Payer organizations are grappling with improving operational efficiency, reducing the cost of care for members, and delivering personalized customer experiences. This, in turn, has led to a growing emphasis on preventative care and a greater need for personalization in the member, physician, and operator experience. Consequently, healthcare payers are striving to adopt the latest technologies to be future-ready and achieve long-term efficiency.
Digital native payers are stealing market share from traditional payers by creating simpler consumer experiences.
The positive is that we are now ready with technology powered by artificial intelligence (AI) to speed up this transformation journey.
Understanding Generative AI
Generative AI refers to a branch of artificial intelligence (AI) that focuses on creating and generating new content or data. While traditional AI methods primarily analyze patterns and make predictions based on existing information, generative AI goes a step further by creating new content resembling patterns in the training data. It is important to note that generative AI models are not limited to content generation alone. They can also be utilized for tasks such as data imputation, anomaly detection, and generating synthetic data to protect privacy. These applications bring numerous benefits to healthcare payers.
Key Benefits and Applications of Generative AI in a Healthcare Payer Ecosystem
Generative AI holds significant potential in yielding cost savings for health insurance companies through various means, such as minimizing fraud-related losses through early detection, enhancing efficiency in claims processing, optimizing resource allocation, providing personalized care and disease management, and improving customer services to deliver greater value. However, it is important to acknowledge that the actual cost savings achieved through implementing generative AI may vary depending on specific use cases, data availability, and the maturity of AI systems.
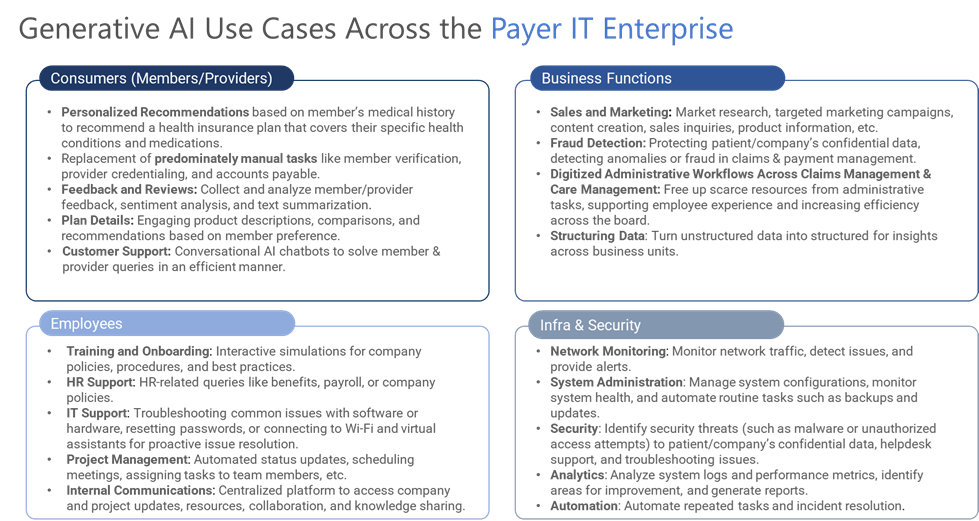
Healthcare payer executives recognize the transformative impact of generative AI on enterprise intelligence. Top health insurance companies are embracing ‘forward-thinking strategies’ that leverage technological advancements to integrate and analyze diverse types and sources of data, often utilizing scalable, cloud-based technologies seamlessly and securely. Yet, the adoption and implementation of generative AI can differ across healthcare payers, with its utilization varying based on specific use cases and organizational priorities.
Unlocking Cost Savings Through Administrative Simplification with Generative AI
Administrative tasks account for a quarter of all healthcare spending. Health insurers can leverage generative AI to automate various administrative tasks, streamline operations and improve efficiency. Here are a few examples:
| Task | Generative AI applications | Benefits | Cost Savings |
| Claims Processing Automation | By training generative AI models on historical claims data, insurers can automate the extraction of relevant information from claim forms, verify the accuracy of the data, and automate the decision-making process for claim approvals or denials. | · Reduced manual efforts · Faster claims processing cycle · Improved accuracy | Savings of ~ 7% to 9% of their total costs (amounting to $80Bn to $110Bn) for private health insurers |
| Document Digitization and Extraction | Training models to recognize and extract key data points from large volumes of paper-based or unstructured documents, such as medical records, invoices, and eligibility forms. | · Time & resource savings | |
| Customer Service Chatbots | Generative AI-powered chatbots can handle routine customer service inquiries, such as policy inquiries, claims status updates, and general information requests. By understanding natural language queries, the chatbots provide accurate and timely responses and offer support to insured members 24/7. | · Reduced burden on human agents · Improved response times · Enhanced customer satisfaction | |
| Provider Network Management | Assist in automating provider credentialing, contract management, and network optimization tasks by analyzing provider data, identifying eligible providers based on specific criteria, and optimizing network configurations. | · Ensure compliance · Improved quality and efficiency of healthcare delivery | |
| Fraud Detection & Prevention | Analyze claims data, historical patterns, and network behavior to identify potentially fraudulent activities. By training models to detect anomalies and patterns indicative of fraud, insurers can automate the fraud detection and prevention process, saving significant costs associated with fraudulent claims and protecting the integrity of their systems. | · Significant cost savings associated with fraudulent claims · Protecting the integrity of their systems | |
| Compliance Monitoring | Assist in automating compliance monitoring by analyzing data and identifying potential non-compliance issues. By training models to recognize patterns of non-compliance, insurers can proactively monitor and address compliance issues, ensuring adherence to regulations and avoiding penalties | · Proactively monitor and address compliance issues · Ensuring adherence to regulations and avoiding penalties |
Navigating the Roadblocks
Implementing generative AI in healthcare payer organizations comes with its share of challenges, including data privacy and security, data quality and bias, interpretability and explainability, ethical and legal considerations, integration and adoption, and regulatory compliance. Addressing these challenges requires a collaborative, multidisciplinary approach involving healthcare professionals, data scientists, legal experts, and regulatory bodies.
On the contrary, payer CIOs have recognized the potential power of AI and analytics in their organizations. However, they often struggle to drive impactful AI adoption due to various factors such as:
- Lack of alignment between AI execution and overall enterprise strategy
- The absence of a clear AI vision
- Fear of missing out, rushing into AI implementation without careful planning
- Organizational bias and misperceptions
- Focusing on one-off AI solutions without a comprehensive AI strategy or governance framework
- Discounting the current state of AI
Addressing these inhibiting factors requires a strategic approach, clear communication, organizational alignment, continuous education, and a commitment to building an AI-ready culture within the healthcare payer ecosystem.
Paving the Way for Generative AI Through Collaboration
In today’s rapidly evolving landscape, it is crucial for healthcare payers to embrace change and remain adaptable and agile to meet emerging needs. By collaborating with technology partners or IT service companies that specialize in the implementation and utilization of Generative AI, healthcare payers can expedite the adoption of a future-proof AI strategy.
Early adopters of AI in the healthcare space are reaping the benefits in terms of patient care and adding to their bottom-line results.
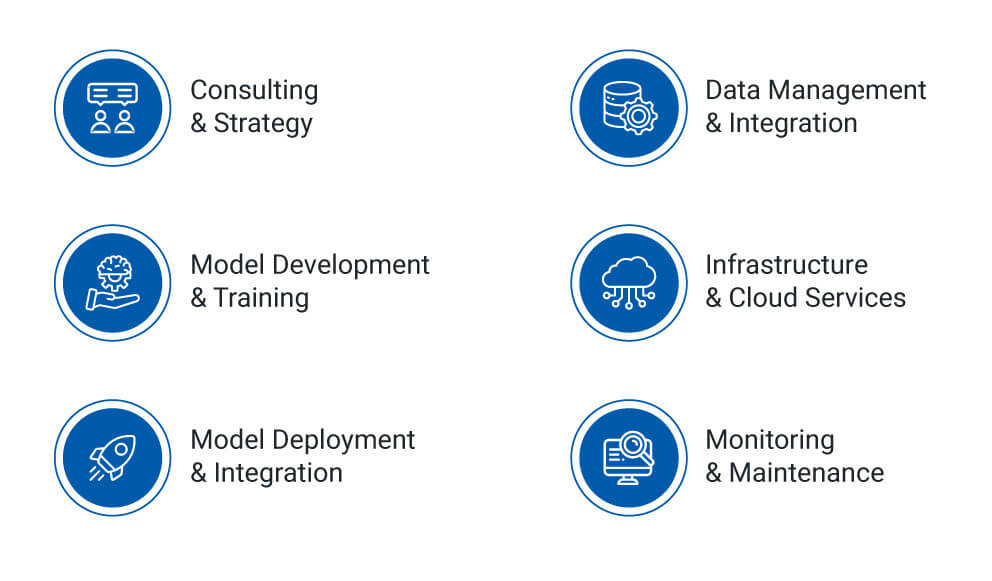
At Hexaware, we offer a comprehensive suite of services designed to support healthcare payers throughout their AI journey. From strategy development to implementation and maintenance, we provide end-to-end support, ensuring that organizations effectively harness the power of generative AI while addressing critical considerations such as data security, compliance, and ethical guidelines.